Dysautonomia: When the Autonomic Nervous System Malfunctions: Postural orthostatic tachycardia syndrome (POTS), neurocardiogenic syncope and more +VIDEO {Lifestyle Medicine}
Dysautonomia–When the Autonomic Nervous System Malfunctions: Postural orthostatic tachycardia syndrome (POTS), neurocardiogenic syncope and more.
{Lifestyle Medicine}
Dysautonomia refers to a group of several different medical conditions that cause an abnormality in the function of the autonomic nervous system. People with various forms of dysautonomia have trouble regulating some or all of the largely “automatic” functions of the autonomic nervous system, which can result in lightheadedness, fainting, unstable blood pressure, abnormal heart rates, malnutrition and more.
Subscribe to my YouTube Channel for more healthy recipes, lifestyle tips and more!
Affiliate Disclosure & Privacy Policy (please review our complete policy here): we use affiliate links and analytics on our website, social media posts and newsletter which utilize cookies placed on your browser to track sales activity. This post is NOT sponsored. When you click an affiliate link on our Website, a cookie will be placed on your browser to track sales activity. When you click these links and purchase a product, we may receive a small commission to help support the maintenance of our website, but the price is the same for you. Users can control the use of cookies at the individual browser level. Please review our complete privacy policy here. Thank you for your support! These statements have not been evaluated by the FDA and should not be considered medical advice or treatment. Please consult your personal health provider before making any changes to your diet or lifestyle.
This post is part 2 of a series. For a general Overview of the Autonomic Nervous System check out part 1 here and check out the Survival Kit for Dysautonomia Management in part 3 here!
Dysautonomia and Autonomic Dysfunction
The autonomic nervous system is composed of three major divisions: the sympathetic and parasympathetic branches and the enteric nervous system. Together, these control the “automatic” functions of the body that you do not consciously think about, such as heart rate, blood pressure, digestion, dilation and constriction of the pupils of the eye, kidney function, and temperature control.
Disorders of the autonomic nervous system can affect any body part or process and may be reversible or progressive. Disorders contributing to autonomic insufficiency or failure can originate in the peripheral or central nervous system and may be primary or secondary to other disorders. These disorders may affect the functioning of the heart, bladder, intestines, sweat glands, pupils, and blood vessels.
Although often missed, dysautonomia impacts over 70 million people worldwide.
Common Causes of Dysautonomia
Primary dysautonomia can result from several different inherited or degenerative neurologic diseases.
Secondary dysautonomia occurs from a variety of causes or processes that damage autonomic nerves or parts of the brain that help control body processes including:
- diabetes
- multiple sclerosis
- HIV/AIDS
- celiac disease
- Sjogren’s syndrome, rheumatoid arthritis, lupus, antiphospholipid syndrome, chronic inflammatory demyelinating polyneuropathy and other autoimmune disorders
- Ehlers Danlos Syndrome
- Mast Cell Activation Disorders
- craniocervical instability
- Chiari malformation
- Guillain-Barré syndrome
- Crohn’s disease and ulcerative colitis
- Lyme disease
- mitochondrial dysfunction
- amyloidosis
- sarcoidosis
- paraneoplastic syndrome
- toxicity
- Parkinson’s disease
Dysautonomia can also occur due to deficiencies or imbalances of certain vitamins, including vitamins E, B1 (thiamine), B3 (niacin) B6 (pyridoxine), and B12 which are essential to healthy nerve function.
Forms of Dysautonomia
Some of the forms of dysautonomia include:
- postural orthostatic tachycardia syndrome (POTS)
- neurocardiogenic syncope
- orthostatic intolerance
- multiple system atrophy
- familial dysautonomia
- baroreflect failure
- autoimmune autonomic ganglionopathy
- dopamine beta-hydroxylase deficiency
- pure autonomic failure
- and more.
Common Signs & Symptoms of Dysautonomia
The potential symptoms of dysautonomia are numerous and vary widely for each individual. In general, symptoms result from inefficient or unbalanced efferent signals sent via the sympathetic and/or parasympathetic systems (click here for an overview of the autonomic nervous system and its various components).
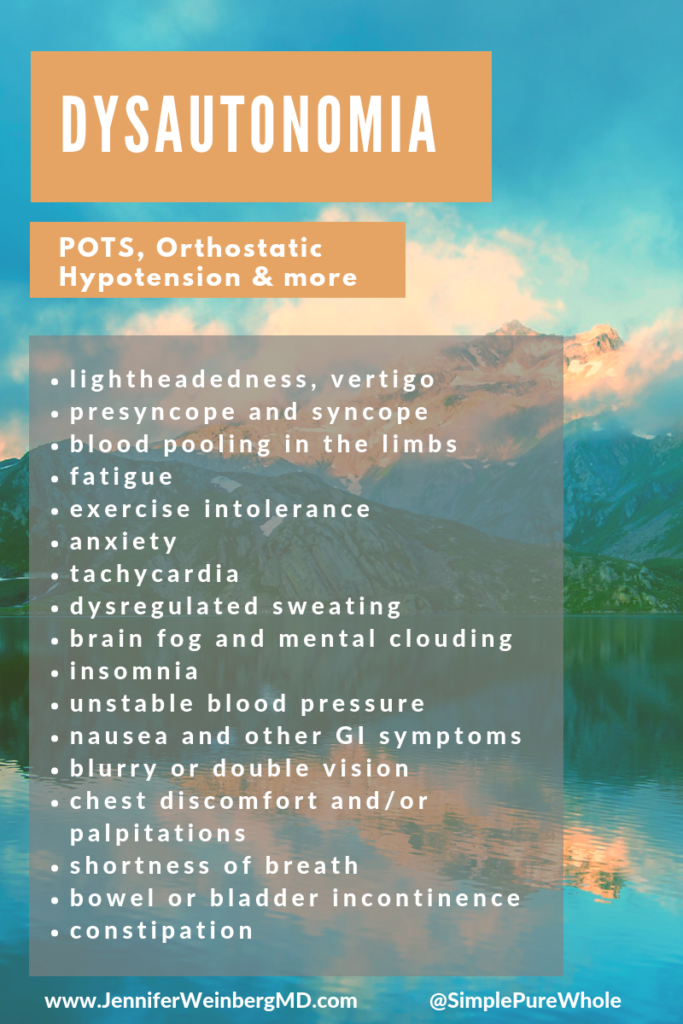
Common symptoms of dysautonomia include:
- lightheadedness, vertigo and dizziness
- presyncope and syncope (passing out)
- difficulty standing still due to blood pooling in the limbs
- fatigue
- exercise intolerance
- anxiety
- tachycardia (increased heart rate)
- decreased, increased or dysregulated sweating
- brain fog and mental clouding
- insomnia
- unstable blood pressure including orthostatic hypotension
- nausea and other GI symptoms
- blurry or double vision
- chest discomfort and/or palpitations (racing heart or feeling of missing beats)
- shortness of breath
- bowel or bladder incontinence
- constipation
Diagnosis of Dysautonomia
There are various tests that can be used to access autonomic function. These may include measuring heart rate and blood pressure in various positions utilizing a tilt table test, sweat testing and other investigations. The diagnosis of dysautonomia depends on the evaluation of the overall status of autonomic functions including investigating cardiovagal, adrenergic, and sudomotor functioning.
Have you experienced dysautonomia?
What do you wish people were more aware of about dysauotnomia?
References:
Bakkers M., Faber CG., Drent M., Hermans M.C.E., van Nes S.I., Lauria G., De Baets M. & Merkies I.S.J. (2010). Pain and autonomic dysfunction in patients with sarcoidosis and small fibre neuropathy. J Neurol. 257(12):2086-2090.
Bilora F., Biasiolo M., Zancan A., Zanon E., Veronese F., Manca F., & Sartori M.T. (2012). Autonomic dysfunction and primary antiphospholipid syndrome: a frequent and frightening correlation? Int J Gen Med. 5:339-343.
Flabeau O, Meissner WG, Tison F. (2010). Multiple system atrophy: current and future approaches to management. Ther Adv Neurol Discord. 3(4):249-63.
Gibbons C.H., Freeman R. (2005). Autonomic neuropathy and coeliac disease. J Neural Neurosurg Psychiatry. 76:579-581.
Goldstein D.S. (2015). Dysautonomia in Parkinson’s disease: Neurocardiological abnormalities. Compr Physiol. 4(2):805-826.
Griggoriou E., Boris J.R., Dormans J.P. (2015). Postural orthostatic tachycardia syndrome (POTS): Association with Ehlers-Danlos Syndrome and orthopaedic considerations. Clin Orthop Relat Res. 473(2):722-728.
Grubb B.P. (2008). Postural Tachycardia Syndrome. Circulation. 117: 2814-2817.
Hall WD. (199). Chapter 75: An overview of the autonomic nervous system. In Walker HK, Hall WD, Hurst JW (Eds.), Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd edition. (1990). Boston: Butterworths.
McLeod KA. (2001). Dysautonomia and neurocardiogenic syncope. Curr Opin Cardiol. 16(2):92-6.
Reichgott M.J. Chapter 76: Clinical evidence of dysautonomia. In Walker HK, Hall WD, Hurst JW (Eds.), Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd edition. (1990). Boston: Butterworths.
I would love to have you in my Insider’s Community! Join for free and receive your FREE Chapters from The Whole Cure: 52 Essential Prescriptions to Overcome Overwhelm, Reclaim Balance and Reconnect with a Life You Love! You can pick up a full paperback or Kindle copy on Amazon for a wealth of insights, exercises and complete toolkit to help you uncover your true passions, authentic purpose and calm confidence as well!
To keep building your healthy lifestyle and best self through everyday habits, take the next step today to commit to a life you truly love and feel fully alive!
-
Pick up a copy of The Whole Cure to build resilience and manage stress in a way that makes life flow with greater ease and joy!
-
Access guided relaxation exercises utilizing the power of the breath and mind here.
-
Join my next online group Whole Cure Lifestyle Transformation Programs to build more powerful coping strategies and skills for meaningful stress management and a calmer life! Contact me to form your own guided online group or register for the next scheduled online program!
Medical Disclaimer: Information provided in this post and related resources are for informational purposes only. Jennifer Weinberg is not providing medical advice, diagnosis or treatment information. The information is NOT intended as a substitute for the advice provided by your physician or other healthcare professional. Every body is unique so be sure to check with your healthcare professional before making any dietary or lifestyle changes taking any medication or nutritional supplement or using any treatment for a health issue. Do not use this information provided for diagnosing or treating a health problem or disease. If you suspect you have a medical problem please contact your healthcare provider promptly and do not disregard professional medical advice based on anything on this website. This website and related resources are not intended to diagnose, treat, cure or prevent disease and do not create a doctor-patient relationship between you and Jennifer Weinberg. These statements have not been evaluated by the FDA. These products are not intended to diagnose, treat, cure, or prevent any disease.
This post was shared with: Saturday Sharefest Home Matters Link Party


Comments
Stacey Horrocks
Thank you for this image. I post it very often in long covid fb groups. I wish that the majority of focus wasn’t always on POTS and fitting in the typical number box that some cardiologists do know. I wish that many other doctors were aware of dysautonomia’s. Its really tough having experienced it myself, and never getting help, vs what my youngest sons experience had been by luck. Seeing that so many cardiologists, neurologists, and others seem unaware of this being illness triggered, if aware of it at all, is sad. So many in covid groups are told what they are experiencing is all in their head, because their lungs or heart checked out fine. Anyway, I appreciate this image, to be able to share. I wish I knew that my oldest son and I could get help for our cases, and that my youngest had not decided he never had it, and rejects the most basic of care and check ups (20yrs old now) because he had one of the very best pediatric cardiologists for his case and experienced remission. Then was allowed off med, and got very sick, and sadly his memory and thinking is also affected so he doesnt even remember the remission year suddenly at age 16, after 8 yrs of symptoms, and having just been diagnosed due to HEDS diagnosis and referral, just a year before. His Dr. was Dr. Jeffery Boris, and he was a diamond of a doctor in CHOP in PA. I learned so much of what a good doctor is, that really cared, thought outside of the box, took time and listened to his patients. He also never stopped researching.
Dr. Jennifer L. Weinberg, MD, MPH, MBE
Thank you for taking the time to leave a comment Stacey! I am sorry you and your family have had to experience these things. I appreciate you sharing my work and your feedback. So glad that you found it appropriate and helpful! I really appreciate your support.